It has been estimated that up to 95% of the current population is suffering from leaky gut syndrome, and many people may not even know that they have it.
Many in the medical community have yet to officially recognize this a medical diagnosis, however, it is believed to be a condition where the lining of the small intestine becomes more permeable, allowing harmful substances such as bacteria, toxins, and undigested food particles to enter the bloodstream and cause inflammation throughout the body. We now know that chronic inflammation contributes to chronic illness and thus not only preventable but reversible.
Leaky gut can be the reason for the following:
chronic diarrhea,
constipation,
bloating, gas,
stomach pain, fatigue,
food sensitivities.
brain fog,
skin rashes,
joint pain,
cardiac disease
thyroid dysfunction
and autoimmune issues.
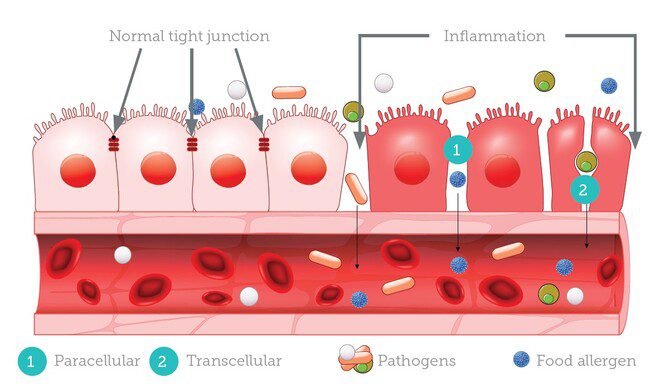
The leaky gut is the result of a breakdown of the intestinal barrier that normally regulates the exchange of substances between the gut and the bloodstream. The lining of the small intestine is composed of epithelial cells that are tightly packed together and joined by tight junctions, which act as gatekeepers to regulate the flow of nutrients, water, and electrolytes into the bloodstream while preventing the entry of harmful substances, such as toxins, bacteria, and undigested food particles.
Leaky gut, also known as intestinal permeability, is a condition where the lining of the small intestine becomes more porous or permeable, allowing harmful substances such as bacteria, toxins, and undigested food particles to leak through the intestinal wall and into the bloodstream.
When these harmful substances enter the bloodstream, they can trigger an immune response, causing inflammation throughout the body. This can lead to a variety of symptoms, including bloating, gas, abdominal pain, food sensitivities, skin rashes, fatigue, and joint pain.
The exact mechanism underlying this increased permeability is not yet fully understood, but it is thought to involve a complex interplay of factors, including genetics, diet, stress, and the gut microbiome.
Some of the factors that have been implicated in the pathophysiology of leaky gut include:
Disruption of the gut microbiome: An imbalance of gut bacteria, known as dysbiosis, can alter the composition of the gut lining and affect the tight junctions, leading to increased permeability.
Dietary factors: Certain dietary components, such as gluten, processed foods, and sugar, have been shown to increase gut permeability by damaging the gut lining.
Stress: Chronic stress can activate the sympathetic nervous system, which can cause changes in the gut lining and increase intestinal permeability.
Medications: Some medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) and antibiotics, have been shown to disrupt the gut microbiome and increase gut permeability.
Environmental toxins: Exposure to environmental toxins, such as pesticides and heavy metals, can also contribute to gut permeability by damaging the gut lining.
An untreated leaky gut will not only lead to nutritional imbalance but can cause widespread inflammation – ultimately causing chronic disease with the risk of premature death.
How to diagnose it:
There is no single definitive test to diagnose leaky gut, but there are a few methods that can help identify the condition:
Symptom analysis: A patient may report experiencing symptoms associated with leaky gut, including chronic diarrhea, constipation, bloating, gas, stomach pain, fatigue, and food sensitivities.
Laboratory testing: check for elevated levels of certain antibodies or inflammation markers in the bloodstream.
This can include the following:
C-reactive protein (CRP): A marker of systemic inflammation that may be elevated in individuals with leaky gut.
Erythrocyte sedimentation rate (ESR): Another marker of inflammation that may be elevated in individuals with leaky gut and other inflammatory conditions.
Anti-gliadin antibodies (AGA): Antibodies that may be elevated in individuals with gluten sensitivity or celiac disease, both of which can contribute to leaky gut.
Anti-endomysial antibodies (EMA): Antibodies that may be elevated in individuals with celiac disease.
Vitamin and mineral levels: Deficiencies in nutrients such as vitamin D, zinc, and iron may be associated with leaky gut and other gastrointestinal conditions.
Additionally:
Intestinal permeability tests: These tests are designed to measure the level of gut permeability by checking for the presence of certain substances in the urine after drinking a solution containing the substance. One test involves drinking a solution that contains two sugar molecules and then collecting urine samples to measure how much of the sugars are excreted. If high levels of the sugars are present in the urine, it may indicate that the intestinal lining is more permeable.
The zonulin test is a laboratory test that measures the level of zonulin in the blood or stool. Zonulin is a protein that regulates the tight junctions between cells in the lining of the small intestine, which control the permeability of the gut barrier.
Finally:
Stool tests: Stool analysis can also be useful in assessing the health of the gut microbiome and checking for imbalances in bacterial populations and the efficiency of the digestive process.
The treatment of leaky gut syndrome typically involves addressing the underlying causes of the condition and supporting the healing of the gut lining. Here are some strategies that may be helpful:
Identify and remove triggers: Work with a healthcare provider to identify and remove any dietary or lifestyle factors that may be contributing to gut inflammation, such as processed foods, alcohol, and chronic stress.
Improve nutrient intake: Focus on nutrient-dense, whole foods that support gut health, such as bone broth, fermented foods, and vegetables. Supplementing with vitamins and minerals that support gut healing, such as zinc, vitamin D, and omega-3 fatty acids, may also be helpful.
Repair the gut lining: Certain supplements, such as L-glutamine, probiotics, and digestive enzymes, may help repair and strengthen the gut lining. However, the effectiveness of these supplements varies among individuals, so it’s important to work with a healthcare provider to determine the appropriate supplements for your specific needs.
Manage underlying conditions: Addressing underlying conditions such as SIBO (small intestinal bacterial overgrowth), autoimmune disorders, and chronic infections may help alleviate leaky gut symptoms.
Manage stress: Chronic stress can exacerbate gut inflammation, so finding ways to manage stress, such as meditation or yoga, may help improve gut health.
In all cases, if you suspect a leaky gut, consult with a practitioner that clearly is open to evaluating this condition and not only knows what to look for but can guide you in the management process. Understand it may take months before you get a complete relief of your symptoms as the root cause has been effectively treated. This may require multiple changes in the approach as every patient is different. Truthfully, think of it as an experiment and both you and the practitioner are the investigators of your health.


